My first podcast has been released by Nurse & Midwife Support to coincide with RUOK Day.
It’s about suicide and nurses and mental health and social media and stuff.
You can access it by clicking here, or on the picture below, or go straight to the platform of your choice: SoundCloud + Apple + Spotify + PodLink
Many thanks to Mark Aitken at Nurse & Midwife Support for interviewing me back on 10th October 2019 (World Mental Health Day) for this podcast.
For those who don’t listen to podcasts, below is a copy of the transcript that I have pirated from this webpage:
Mark Aitken: I’m at the Australian College of Mental Health Nurses 45th International Conference in Sydney. My guest today is Paul McNamara: Clinical Nurse Consultant, Consultation Liaison Psychiatry Service at Cairns and Hinterland Hospital and Health Service. Welcome, and hello Paul!
Paul McNamara: G’day Mark, thanks for having me.
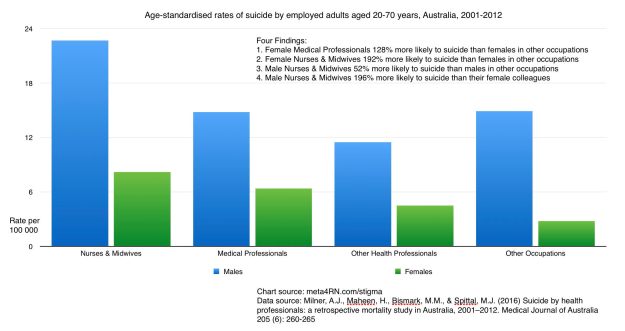
MA: It’s great to have you here today Paul. Today, we will discuss suicide and support for nurses, midwives and students at risk of suicide and following the death by suicide of a colleague. Paul, as you report in your blog on your website (meta4RN.com which I’ll get you to talk about shortly) you cite a retrospective study into suicide in Australia from 2001 to 2012 that uncovered these alarming four findings:
- Female medical professionals are 128% more likely to suicide than females in other occupations.
- Female nurses and midwives are 192% more likely to suicide than females in other occupations.
- Male nurses and midwives are 52% more likely to suicide than males in other occupations.
- Male nurses and midwives are 196% more likely to suicide than their female colleagues.
They’re incredible statistics. Quite disturbing I think, Paul. Would you please tell our listeners a bit more about that? But also, your role and meta4rn.com and why you wrote the blog about suicide that you’ve titled Nurses, Midwives, Medical Practitioners: Suicide and Stigma.
PM: Sure. The hospital that I work in, I’ve been there off and on for nearly 20 years now. Back in the early 2000’s three of the nurses who worked there died by suicide. That was a bit of a shock to us all. It happened within a fairly short amount of time, about 18 months I think it was. It felt like knock, after knock, after knock. A lot of us, myself included, were standing around looking at each other. Looking at our colleagues on the nursing team and thinking, “Oh Christ, what could we have done better? What could we have done differently?” That’s really stuck with me. Then with my role, I work as a mental health nurse in the general hospital. Not everyday day of the week, but certainly every week of my working life I will see people who have attempted to take their own lives and have survived it and been admitted (medically or surgically) to be patched up. While that’s happening, I’m providing the mental health input.
I guess that suicide is just an everyday part of my working life. A bit more than I would like, sometimes, to be honest. When it effects my colleagues, that gives it an extra resonance. It was with those thoughts bouncing around my head when I saw that paper come out with that data. That was published in November 2016, it was written by a pretty impressive bunch of people. They were all doctors on the team. I think one of them was a PhD doctor, not a medical doctor, but the rest of them were medical doctors from various specialties. The bits of that story that were picked up by the mainstream media were about the escalated risk to doctors of suicide. The mainstream media didn’t really pick up on the escalated risks to nurses and midwives, which were actually a bit higher than the risks for female doctors. Interestingly, male doctors don’t kill themselves at a greater rate than blokes in other professions. So, it was very much about nurses and midwives. As we know, most nurses and midwives are females. The whole thing has just got a bit of a resonance for me. It worries me. I guess the title that I gave it, it was speculative. I wonder about the stigma around suicide as we (nurses and midwives) get exposed to suicide stuff so much. I wonder whether we stigmatise ourselves around that. That was what the blog post was all about.
MA: Thanks Paul, I think you make some really interesting points there. Would you tell our listeners a bit about meta4rn.com? People will obviously want to access this blog once they listen to this podcast. I think it’s a really important blog, so what is it and why did you start it?
PM: This could be the cleverest thing here today Mark..
-Laughs-
MA: Apart from us.
PM: That’s right. Meta4rn.com is a homophone, it’s a bit of a play on words. It can be read two ways: metaphor, as in using an analogy to get a point across. A lot of education happens that way, where we use metaphors. I think particularly amongst nurses and midwives, you’ll be at a nursing station saying, “You do it this way because it’s a bit like a…” We use that kind of language a lot. We use metaphors a lot, and I threw on RN at the end because that’s what I am, an RN. Another way to break down that name is meta, which is like if we were having a conversation about another conversation. That would be a meta conversation. A lot of the stuff I talk about on the blog is a conversation about nursing conversations. That was where the idea for the name came from. Every now and again, I feel a bit self-conscious about it because it is a little bit wanky.
I came about setting up that blog because at the time I was working in perinatal mental health. By definition, my patients were women aged somewhere between 15 and 45. That demographic had the best and quickest uptake of social media and smartphones. This is going back to 2009/2010 when I first started mucking around in that space. If you remember back to then, iPhones were still a relatively new idea. I think they had been on the market in Australia for a year and a half, two years. It was women within that age bracket who were buying them first using social media the most. I was saying to the organisation that I was working for at the time that we, as perinatal mental health, should be getting in that space where the women are. But it was a government organisation, bureaucracies are a little bit sluggish. They didn’t really want to act on that, so I left the organisation behind and just set it up representing myself as a nurse (not the organisation). But I put myself up on social media in that space. Initially, because I was still working in perinatal mental health, it had a focus around that. But the funding for that role disappeared, so my focus has become much broader since then.
MA: It certainly has grown, as has your following. You’ve got a lot of subscribers to your website and I get regular emails and information.
PM: Yes.
MA: If people want to subscribe they can just google meta4rn and they can become a subscriber to your site and get access to some of the great information on your blog?
PM: Yes, and look, only if you want to. It won’t be too spamy, I tend to write about one blog post a month now. So, you can do that. If you don’t want to subscribe, if you’re like me you’re probably sick to death of too many emails. Just have a look around and see if there’s anything of interest for you.
MA: Navigate it via the website?
PM: Yes.
MA: You’re an excellent speaker about the importance of nurses and midwives blogging, or being active on social media. Indeed, Paul and I are at the 45th International Mental Health Nurses Conference in Sydney. We have been here since the beginning of this week. We’re recording this podcast on the 10th of October which many of you will know is World Mental Health Day. So, happy World Mental Health Day to you all! May you commit to your own mental health self-care and support. Paul, I think that’s vital. You gave a great session yesterday about nurses and social media. Could you talk a bit more about that please?
PM: The session was 45 minutes long so I definitely won’t give you that much information. But look, the short story is that we (as nurses and midwives) now have access to telling our stories and more access to the public conversation than what we have ever had before. I used some data to back this up, so it’s not just a dopey opinion. But I think maybe if we went back 10 years in time it would be frustrating to hear mainstream media talking about nursing issues without actually talking to any nurses. That still happens now, of course. But, from my point of view, I think that rather than getting frustrated about the mainstream media why don’t we take control of what we do have? This is things like social media; Twitter, blogs in particular, YouTube, Facebook. Make it separate from your personal accounts. I find Instagram a little bit harder to use in a professional sense, but I’m playing with it. I’m probably the wrong demographic to really be good at Instagram. All of these social media platforms are free to access and give us the opportunity to get our voice out there and join in on those conversations. People get to hear from us now, whether they want to or not. I think that’s a really important power. I think that we’d be foolish to ignore it.
I’m not suggesting for a moment that each and every nurse, midwife or student listening to this podcast should go out and create a social media portfolio. That’s not going to be everybody’s cup of tea. But there were some people who were wondering about it, and I would encourage you to explore that space. Nurse Uncut, the NSW Australian Nurse and Midwifery Foundation companion website, they’ve got a blog role there that includes some great examples of nurses and midwives who have got blogs out there. Some of them are really really good, many of them are much better than mine in terms of the way that they look and the clarity of information that they present. But I think that if you’re thinking of having a go, have a go. My only suggestion or caution around that, as a mental health nurse so of course we’re big on boundaries, if you are going to go and do that be really intentional about setting up a professional social media portfolio quite separate to your personal stuff. So, my holiday snaps and what have you, to show off to family and friends are not under my own name. You wouldn’t be able to stumble across them easily, but if you were to Google Paul McNamara mental health nurse or Paul McNamara Cairns you will get bombarded with stuff that I want you to see. I’m mindful that some of my patients, colleagues and bosses will search for me on Google. Usually not with sinister intent, but more out of curiosity. I want to be in charge of what they see, and that’s what that’s all about.
MA: Thanks Paul, I think that’s really useful information. It’s a bit outside of our key or core topic today but it’s still some very useful information for nurses and midwives. Also, I would add that there’s some very useful information on using social media and blogging effectively. But also, in relation to your regulatory requirements on the Nursing and Midwifery Board of Australia website. So, if you’re kind of worried about how you’re presenting yourself, check those out first to make sure that you’re considering the regulatory requirements of your registration.
PM: And, look, I feel like those are fairly common sense guidelines. The short version is: don’t be a dick, and you’ll be fine.
MA: Good point Paul. Paul, you and I have been speaking about suicide and our concern for the profession, for nurses and midwives in relation to this since we first spoke at the beginning of Nurse & Midwife Support in 2017. In fact, you contacted me and raised your concern in relation to this issue. Indeed, the effect that the suicide of several colleagues at your health service had on you and other members of the team. Would you please share with our listeners why you think this issue is important for us to discuss? In relation to nurses and midwives? Indeed, getting it out into the open.
PM: I was really thrilled when Nurse & Midwife Support launched. I don’t know whether it’s a coincidence that that launch in March 2017 coincided with that paper I was talking about, which was published in November 2016. It was probably too short a lead time to have caused an effect, but the timing was great anyway. The advantage that Nurse & Midwife Support have over the Employee Assistance Programs or going off to see your GP is that it’s specifically targeted to nurses and midwives. It’s 24 hours a day, 7 days a week, which reflects the shift working nature of our jobs. For many and probably most of us anyway. Having that great degree of flexibility is really important.
A downside is probably that it’s all phone based. For a lot of us, at a time of emotional distress we’d really appreciate that face to face contact. But this is a good first step and I’m really pleased that it’s there. I’m the mental health guy who wanders around the general hospital, and I hear mixed reports about peoples experience with the Employee Assistance Program. Some people have had a terrific service, but not all. Particularly, if people are carrying concerns that they think may jeopardize their employment or their registration, accessing support via your workplace is scary. Being able to go beyond the workplace, far far away down to the other end of the telephone has that advantage around that. So, if the way that you manage your stress is that you’re really hitting the booze or doing something that might get you judged poorly in your workplace, I think it’s a great advantage to have somebody far away from the workplace that you can have that conversation with. So, if you do need to go back to your workplace and discuss that part of the issue, you may be able to go back with an at least partially formed solution. I think that that’s the great advantage.
MA: Thanks Paul. Just to clarify for our listeners, Nurse & Midwife Support provides brief intervention counselling and referral pathways. If you phone our service and you need face to face counselling, as Paul suggests, then we’re able to give you some referral options so that you can access that service. But I think in the first instance, it’s often really useful to phone a service like Nurse &Midwife Support, talk through the issue and get some options in terms of where you may go next. Paul, you state in your blog that suicide is a complex matter, that does not lend itself to easy understanding or simple solutions. However, something we know about health professionals is that they know that there are mental health services and supports. Health professionals know that these services can be accessed by people who are feeling suicidal. The data that you cite, and the research suggests that health professionals have an actual or perceived barrier to accessing these existing supports. You posed the question, I wonder what that barrier is? Paul, what is the barrier?
PM: I need to really clarify that I don’t know, that’s probably something for another team of researchers to explore. I can’t pretend that I know for sure but I imagine, through conversations with colleagues, that one of the barriers is about embarrassment. Shame. Nurses and midwives tend to be empathetic creatures, but because we’re so immersed in other people’s traumas we sometimes put up barriers which sometimes include some really irreverent defences. Like, if someone comes in after a suicide attempt, I have heard people say, “Why don’t they do it the proper way?” Stuff like that. When we say stuff like that, in front of each other, it doesn’t really give us permission to disclose that we’re at that point or getting close to being at that point. So, I think that sometimes the defences that we use so that we can go back to our job from day to day may accidentally stigmatize accessing support for each other. That’s what I was really trying to argue in that blog post. That we should just be a little bit careful about the ways in which we talk about suicide, for our patients and/or vulnerable colleagues. Let’s reach out to our colleagues, give permission and actually encourage them to come out and say that it’s ok to put up your hand if you’re going through a really rough spot. It would be foolish to pretend that that alone would make a big difference, but it would help.
MA: Thanks Paul. Do you think that there is a specific stressor, or there are stressors that prompt nurses to commit suicide rather than seeking help?
PM: Again, I’ll throw in the disclaimer that I won’t pretend to have all of the answers. But think about us, as nurses and midwives, and think about our psychopathology. We’ve probably got more empathy than the general man in the street. We’ve been attracted to do a job which almost in essence means that we’ve got to put the needs of others before our own needs. Anyone whose held their bladder for an 8-hour shift would recognise that. While you’re running around putting in catheters for other people, it’s not unusual for us to put the needs of others before us. I wonder whether that’s a part of the reason that nurses and midwives are overrepresented in suicide data, we’re not good at putting ourselves and our own needs first. Throw in on top of that, many of us do shift work so being sleep deprived makes us more emotionally vulnerable. We get exposed to other peoples’ trauma face to face. We’re up close and personal with our patients physical and emotional traumas. We’re the people who go behind the curtain and get exposed to those really raw emotions. For us to pretend that that’s not going to have a knock-on effect, would be a little bit foolish.
MA: Thanks Paul. On this day, World Mental Health Day, the 10th of October, we obviously place the spotlight on mental health. Do you think that there’s a lot of untreated mental health amongst nurses and midwives? Or indeed, untreated mental illnesses amongst nurses and midwives?
PM: Yes, we’re overrepresented in those common mental health problems such as depression and anxiety. We’re more likely than our patients to experience depression and anxiety, and I’m guessing for some of those reasons that I was just talking about before. There is, yes.
MA: Do you think that a more widely utilised facility for clinical supervision for nurses and midwives would improve their mental health and wellbeing?
PM: It’s about the only thing that stopped me from going mad. I probably am still a bit mad, but my clinical supervision has been such an important part of my practice. In Queensland, anyway, clinical supervision has been available to any mental health nurse working in the public sector since 2009. Interestingly, in the guidelines before that which were implemented in 2003 in Queensland, nurses were explicitly excluded from it. The rationale for that was a really good one, which is that it would cost a lot of money. But, it’s really important. We do emotional labour. We need to make sure that we look after ourselves.
Clinical supervision, just for those who don’t know a whole lot about it, it’s a bit of a dopey name. The analogy I use is say, a lot of our listeners will hold a Bachelor of Nursing or a Bachelor of Midwifery. Some of our listeners may hold a masters in this space, but not many of us will actually be bachelors or be masters. So, the name doesn’t necessarily accurately reflect what’s going on now. Clinical supervision was named about 100 years ago by psychotherapists. They were addressing their patients, one on one, who were talking through their problems. If they didn’t feel 100% confident that they weren’t making mistakes with the way that their sessions were progressing, they could tap a trusted colleague on the shoulder and be able to discuss the case with them. The colleague was then able to give supervision and support, to minimize the risk of harm to the patient.
That’s where the name comes from, it’s a bit icky for nurses and midwives. We’ve come from a fairly bullying culture so the idea of supervision sounds like scrutiny. It’s not. It’s very much about support and I was really thrilled to see in April this year that the College of Nurses, the College of Midwives and College of Mental Health Nurses in Australia put out that joint statement saying that Clinical Supervision should be available to all nurses and midwives, not just mental health nurses. All nurses and midwives in Australia should be given that opportunity to reflect on their practice so they can care for themselves. It’s not a self-indulgent thing, as this will enable them to provide better care for their patients.
MA: Thanks Paul. Just to pick up that point you made, because I do hear this when I’m around the traps talking to nurses and midwives around the bullying culture in nursing. I know some of our listeners will be very interested in this.
PM: I’ll be fair dinkum with you about this Mark. I think as a bloke, I kind of have managed to stand apart from that. It’s a bit weird, we’ve got two men here talking about nursing and midwifery. I think 89% of general nurses are female and 99% of midwives are female. So, it’s weird that blokes are talking about this, and I think that as a man I’ve probably dodged most bullets around bullying. But I hear it from my colleagues. A lot of it isn’t necessarily intentional. It’s about what happens in our workplace, we’ve got this busy stuff going on in busy wards that are crisis driven. There’s always a crisis going on. When something that would normally be addressed with empathy, kindness and calmness. Being met with an invitation for tea in the staff room, I think nursing has a culture where it’s like, “I can see you’re upset, but let’s get on with it.” I think that that emotional neglect is probably the biggest source of bullying that I’m aware of. But I know that through my gender, I’ve got blind spots around bullying.
MA: Thanks Paul, and what are you doing to look after your own mental health? A part from clinical supervision?
PM: Well clinical supervision is number one. My wife Stella is also a nurse, so we speak the same sort of language. We kind of look after each other. We’re really good at going to restaurants and going on holidays. We make a point of doing those sorts of things, to give ourselves treats. We’re working to get a benefit out of our nursing work. A personal benefit. More recently, I’ve recommitted myself to being a bad tennis player and an awful guitar player. Bought myself a new tennis racket and a new guitar, and I’m determined to be a little less crap at both.
MA: Well I look forward to seeing you in a band soon Paul. Just one last question, do you have a cut through message that will support nurses and midwives to seek help? Who may be at risk of suicide?
PM: Yes, don’t leave it until it’s too late. I think we’re almost predisposed to go; “Oh she’ll be right, she’ll be right, she’ll be right.” Don’t leave it until it’s crisis point would be my idea. If you’re going through a bit of a rough patch, don’t be shy about picking up the phone to Nurse a& Midwife Support. If you’ve got a decent GP who you can have a yarn to, that would be the next best port of call. He or she can make a referral to a credited mental health professional such as myself or maybe a psychologist or someone who can provide that one on one emotional kind of support. Just prioritise your health. I’m playing a tricky little emotional blackmail on your listeners now, but even if you don’t want to do it for yourself, it would be really good for your patients if you’re not overwhelmed by depression and anxiety. If you’re a bit motivated by helping others, you can do that by helping yourself.
MA: Thanks Paul, great advice. Well I can’t believe we’ve come to the end of another podcast, we could talk about this all day! Thanks Paul, we’ve had some great conversations since we met in 2017. We’ve talked about Nurse &Midwife Support today; mental health, suicide and the barriers for nurses and midwives accessing support. We’ve talked about stigma, the research, we’ve provided some strategies for overcoming stigma and the elements to supporting nurses and midwives at risk of developing mental illness and suicide. Paul, do you have any final words of wisdom for our listeners?
PM: Wisdom? No. But look, good luck out there. We know it’s a difficult job. You deserve to be cared for.
MA: Thanks Paul. If you found this podcast useful, please share it with other nurses, midwives, graduates and students. Feel free to rate us on whatever platform you’re listening on. That will help to elevate us and for other people to actually find our podcasts. This is important, because your health matters. Look after yourselves and each other, we’ll have some information attached to this podcast that will provide you with access to Paul’s blog, his website and indeed some services that can support your health and wellbeing. Take care, and I’ll speak to you next time.
Three Links
The podcast and transcripts:
www.nmsupport.org.au/resources/podcasts/discussing-suicide-jon-tyler-paul-mcnamara
Suicide info:
www.nmsupport.org.au/mental-health/suicide
Nurses, midwives, medical practitioners, suicide and stigma
www.nmsupport.org.au/news/nurses-midwives-medical-practitioners-suicide-and-stigma

End
That’s it. Thanks again to Nurse & Midwifery Support – what a terrific back-up for me and my colleagues.
As always, your feedback is welcomed via the comments section below.
Paul McNamara, 10 September 2020
Short URL: meta4RN.com/podcast

















 Stevie Jacobs is the pen name of a newly-minted Enrolled Nurse. The person behind Stevie is smart, experienced in life and has some awesome insight into the world of the student and new graduate nurse.
Stevie Jacobs is the pen name of a newly-minted Enrolled Nurse. The person behind Stevie is smart, experienced in life and has some awesome insight into the world of the student and new graduate nurse.